Medical science is a rapidly changing and dynamically evolving field of knowledge. This continually fluctuating body of knowledge poses a unique challenge for healthcare instructional designers: How to create the right balance in their curriculum, between learner needs and the vast amounts of available knowledge areas to cover. The answer lies in creating Adaptive Learning (AL) solutions.
Adaptive Learning and Healthcare
Adaptive Learning (AL), which also goes by Technology Enabled Learning (TEL), is a computer algorithm- based learning/teaching approach. The algorithms interact with learners to deliver personalized learning content based on their (learners’) individual learning needs.
In non-adaptive learning settings, an emergency medical services (EMS) employee, for instance, may opt for an eLearning course and realize that he/she breezes through 95% of the EMT-Basics curriculum. However, the algorithms from an AL-based learning program would initially interact with the learner – perhaps through a series of quizzes, online task assignments or questions. Based on the responses/assessment from those interactions, the AL approach presents the learner with an altered curriculum containing more advanced levels of content.
So, instead of cycling through all the EMT-Basics curriculum, the Emergency Medical Technician (EMT) may just have to learn 5% of the basics, and then skip directly into the EMT-Intermediates or the Paramedics learning content.
AL is extremely relevant in healthcare environments, where patient outcomes depend on medical practitioners quickly “getting up to speed” on the latest medical knowledge. While traditional digital learning is great at delivering “on-demand” learning, AL is excellent at adapting the curriculum based on learner needs as opposed to offering learning when and where needed.
AL isn’t just a theoretical concept; it delivers real results in real-world healthcare learning. A survey by the New England Journal of Medicine (NEJM), of 4,400 of its NEJM Knowledge+ platform users, concluded decisively that AL in healthcare does pay dividends. Participants rated AL features of the platform, including content served and relevance of the content (delivery of quiz questions), high on a relative basis.
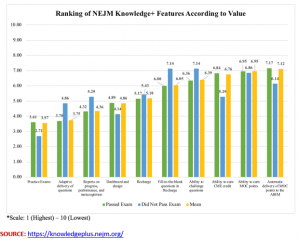
The study also found that 95% of respondents using AL-based learning passed the American Board of Internal Medicine Certifying Examination (ABIM-CE) professional certification on their first attempt. The national average for that accomplishment is 89%.
Creating Adaptive Learning Courses – Step by Step
Creating effective AL-based learning content is a phased approach, which starts with understanding the healthcare learning needs of your stakeholders, and culminates with refining your learning solution. Here’s a 6-step process for developing AL healthcare solutions:
STEP 1: Know Your Sponsors’ Needs
Before you start creating drawing board renditions of your curriculum and courseware, you must understand what it is the course sponsors want. Typically, hospital administrators, Human Resource (HR) specialists and healthcare facility managers see healthcare training needs from a different lens than instructional designers. It is important, therefore, as the first step in instructional design, to understand your sponsors’ needs and priorities.
STEP 2: Know Your Learner’s Needs
Step 1 will give you a broad perspective for building your course. You must now take that macro view, and translate it into learning needs for the front-line healthcare professionals at the institution or organization. Understand what specialties and healthcare disciplines your training content must address.
A good start to Step 2 is by getting to know how various teams – physicians, nurses, ER support staff – work together, and the roles they play in delivering patient care. This last piece of understanding will serve you well in creating detailed scenarios, tests, and simulated exercises – (see Step 4 for more on this)
STEP 3: Plan your Baseline Identification
AL is all about delivering healthcare professionals the unique learning experience that they need, and not what a typical learner “like them” should consume. In order to deliver customizable course curriculums, it is essential that you plan the initial set of interactions that the module or program will have with each learner so that you establish a clear baseline of learning needs.
STEP 4: Develop Specific and Realistic Case Studies and Use Cases
Step 3 will provide you with the learning gap that exists between what a (specific and individual) healthcare professional needs to learn, and the knowledge and skill levels he/she must have to deliver the quality of care expected of him/her. Your case studies and use cases must address that gap.
We’ve all experienced case studies and use cases that, while testing learners on the content presented, don’t really challenge learners for the roles they play in the real world. Your interactions through Steps 1 and 2 will provide you an in-depth understanding of the learning needs your stakeholders want to address. These might include:
- Preparing physicians for Board-level certification
- Equipping X-Ray and CT-scanner equipment operators with the skills needed to better use the machines
- Building in-house capabilities to offer new procedures (surgical actions, therapies, counseling) to patients
The baseline created in Step 3 will highlight learning gaps to fulfill the needs from the initial two steps. Develop case studies and use cases that address those specific learning needs, as opposed to more broad-based or generic healthcare delivery needs.
STEP 5: Use Apps and Technologies to your Advantage
Make sure you choose relevant tools and technologies as part of your AL curriculum. This includes online software simulators, like open-source-based VitalSign Simulator and Patient Monitor. You may also find the use of other tools, such as intelligent manikins, helpful in building AL healthcare learning solutions.
STEP 6: Pay Attention to Assessments
When constructing your use cases and simulated scenarios, consider building them around online software simulators, like those available from vHealthCare. These tools have built-in assessment modules that enable learners to:
- Continually evaluate their knowledge levels and refine their learning
- Alter (gloss through or skip) their learning sequences
- Revisit, review or revise previously completed modules or lessons
- Acknowledge the need for, and benefit from, other learning resources (available externally or within the institutions’ learning program)
Step 6 is likely the heart of any AL-based learning program because this is where instructional designers and medical learning content developers can add “adaptability” to learning.
STEP 7: Review and Refine
The final step, in this 7-step iterative process, is for instructional developers to continually review and refine their own work. Because health sciences are a constantly evolving field, the tools, processes, techniques, and content developed to teach it must also evolve.
As part of Step 6, therefore, be sure to include feedback on the course, the curriculum, and training approaches used. Step 7 must then use that feedback to modify components of the course where necessary.
Continuous Adaptation
The above 7-step process for developing and delivering AL-based healthcare learning mirrors (at a high-level) the 4-phased AL approach proposed by the assistant dean for undergraduate medical education at Vanderbilt University School of Medicine, Dr. William B. Cutrer, MD.
- Planning
- Learning
- Assessing
- Adjusting
While Dr. Cutrer’s 4-phased approach to AL empowers and challenges physicians to become lifelong learners, the step-by-step approach discussed above aims to help instructional designers support that objective. It does so by helping healthcare learning content developers and instructional designers produce personalized learning that help healthcare practitioners improve their existing skills and stay current on emerging medical knowledge.

Leave A Comment